


This article highlights the essential heart failure medications that play a vital role in managing this condition effectively. We explore various classes of medications, including:
Each of these medications has unique roles and benefits that can significantly improve patient outcomes. It's particularly important to consider personalized treatment strategies, especially for our elderly patients, who often face unique challenges in managing heart failure.
Understanding your concerns is our priority, and we want to reassure you that there are effective treatments available. By working closely with healthcare providers, patients can find the right combination of medications tailored to their individual needs. Remember, you are not alone in this journey, and seeking help is a positive step towards better health.
In addition to medication, it's essential to have a supportive care plan in place. This can include:
Together, we can navigate the complexities of heart failure management, ensuring that you feel empowered and supported every step of the way.
We encourage you to reach out to your healthcare provider to discuss any concerns or questions you may have. Your health and well-being are of utmost importance, and there is a community ready to support you.
Heart failure remains a pressing health concern, especially for our aging population. Effective management can truly enhance quality of life, and it’s important to know that you are not alone in this journey. The landscape of heart failure treatment is evolving, offering a variety of medications that not only alleviate symptoms but also reduce hospitalizations and improve overall outcomes. However, we understand that navigating through these options can feel overwhelming for both patients and caregivers.
What essential heart failure drugs can genuinely make a difference in managing this complex condition? Together, we can explore these solutions and find the support you need.
At Amavita Heart and Vascular Health®, we understand that cardiovascular issues can be daunting, especially for our elderly patients who often face unique challenges. Our comprehensive approach integrates advanced medical practices with compassionate support, ensuring that each individual receives the care they deserve. We create personalized treatment strategies tailored to meet the specific needs of every patient, acknowledging that recent advancements, such as the FDA's approval of heart failure drugs like finerenone for cardiac insufficiency with preserved ejection fraction, are reshaping the landscape of care options available.
Our multidisciplinary team is dedicated to providing not just exceptional medical assistance, but also the emotional and educational support that is vital for effective cardiac management. This holistic strategy is particularly beneficial for older adults, who may be managing multiple health conditions. As leading cardiologists emphasize, a tailored approach enhances patient involvement and commitment to treatment, ultimately leading to improved outcomes.
At Amavita, we focus on empowering our patients through education and support, fostering a collaborative environment where individuals feel valued and understood. This commitment to personalized care addresses not only the medical aspects of cardiovascular issues but also prioritizes the overall wellness of our patients. We strive to ensure that they receive the attention and resources necessary for an enhanced quality of life.
If you or a loved one are facing cardiovascular challenges, we invite you to reach out to us. Together, we can navigate this journey towards better health with understanding and compassion.

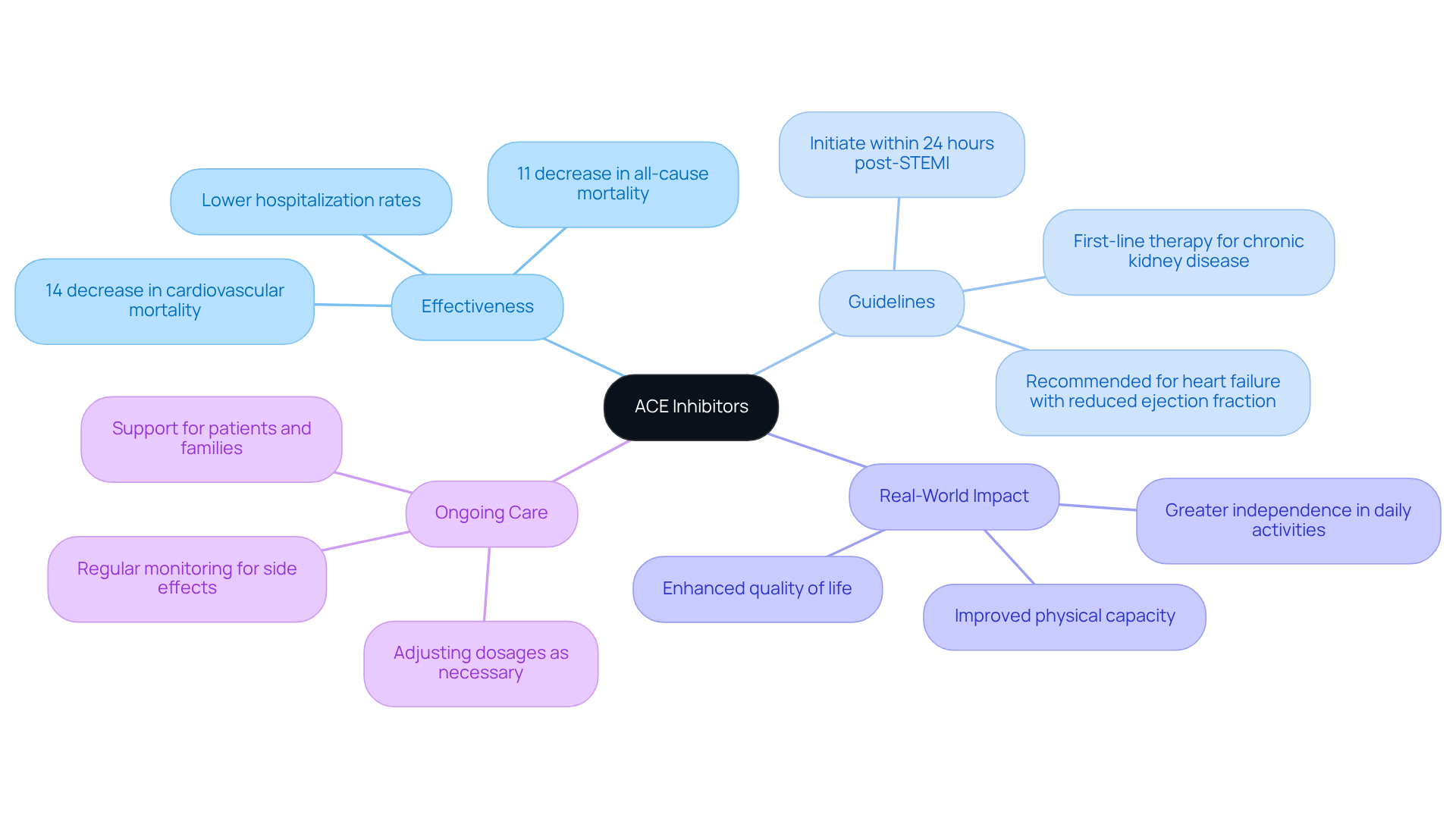
Angiotensin-Converting Enzyme (ACE) inhibitors, like lisinopril and ramipril, are recognized as the primary treatment for managing cardiovascular issues, particularly in older individuals. These medications work by relaxing blood vessels, which helps reduce the workload on the heart and improves blood flow. Recent research indicates that ACE inhibitors are associated with a statistically significant 11% decrease in all-cause mortality and a 14% decrease in cardiovascular mortality among individuals with heart conditions. Moreover, they have been shown to significantly lower hospitalization rates related to cardiac issues, offering substantial benefits in managing this condition.
Current guidelines recommend heart failure drugs such as ACE inhibitors for individuals with heart failure and reduced ejection fraction, especially those with a history of myocardial infarction. This recommendation is crucial, as older adults often face multiple health challenges, making effective management essential for enhancing their quality of life. Real-world examples illustrate how ACE inhibitors have led to improved physical capacity and reduced symptoms, allowing elderly individuals to maintain greater independence and engage more fully in daily activities.
At Amavita Heart and Vascular Health, we prioritize your well-being by integrating advanced imaging and comprehensive evaluations to ensure that high-risk individuals receive tailored cardiovascular care. Our CardioElite™ SNF Program enhances this approach by focusing on reducing readmissions and improving individual outcomes through coordinated care. Regular monitoring is essential to adjust dosages and manage potential side effects, ensuring optimal therapeutic results. By alleviating symptoms and preventing hospital admissions, heart failure drugs like ACE inhibitors play a vital role in enhancing the overall quality of life for older individuals facing cardiac challenges. It’s important for patients and their loved ones to remain vigilant about observing and adjusting treatment as necessary, knowing that support is always available.
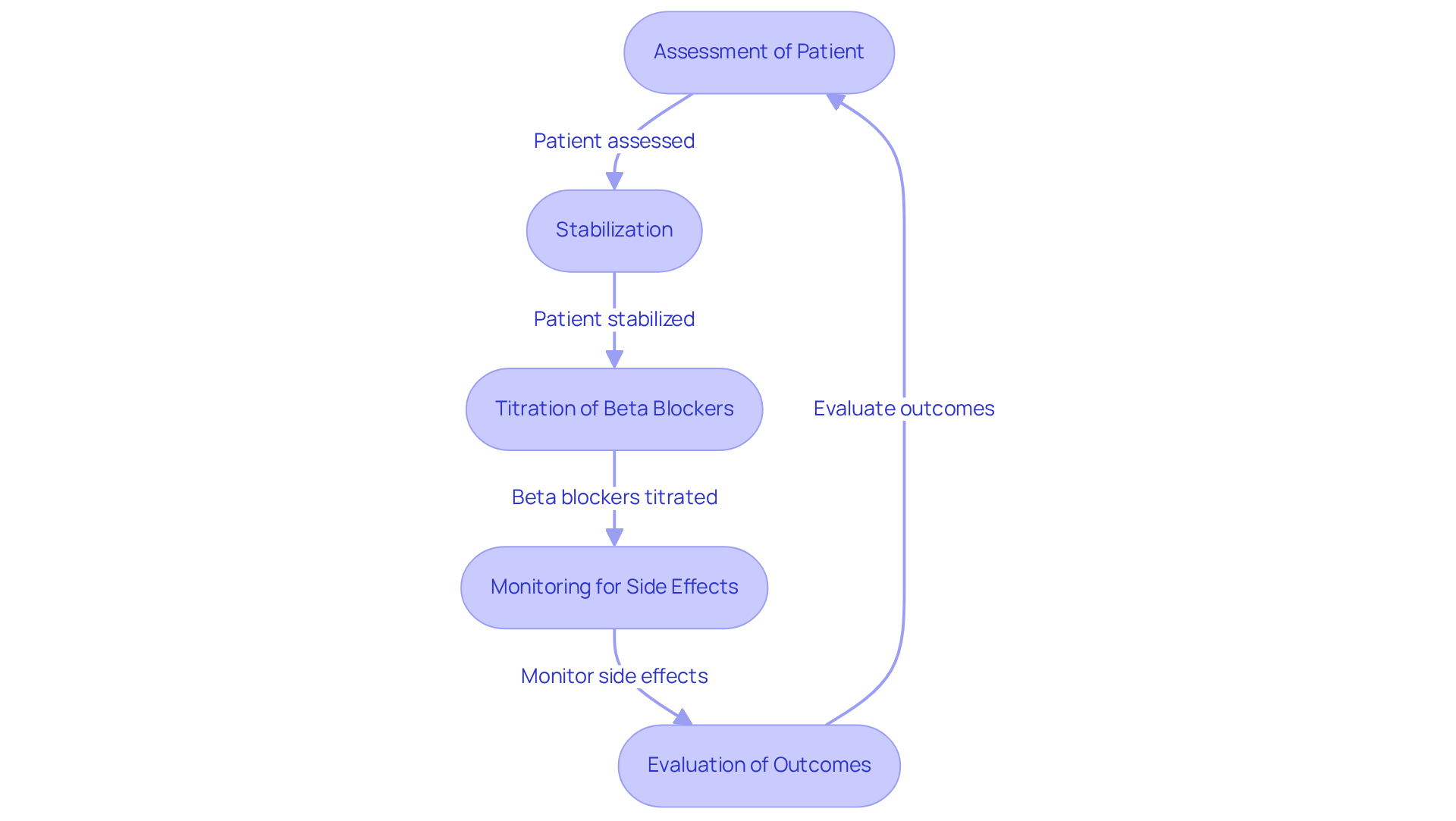
Beta blockers, such as carvedilol and metoprolol, play a crucial role in managing cardiac symptoms, particularly for older individuals. These medications are effective in reducing pulse rate and lowering blood pressure, leading to improved heart function and relief from symptoms like fatigue and shortness of breath. Recent research indicates that heart failure drugs, such as beta blockers, can significantly enhance the quality of life for older adults with cardiac failure, with a meta-analysis showing a 25% relative decrease in all-cause mortality associated with their use.
In real-world scenarios, many older individuals have experienced remarkable improvements in heart function following treatment with heart failure drugs, including beta blockers. For example, a multicenter cohort study revealed that those treated with beta blockers had a 36% reduction in mortality two years after a myocardial infarction, highlighting their effectiveness in this population.
Cardiologists emphasize the importance of careful titration of beta blockers in older patients to minimize potential side effects. As Dr. William E. Chavey notes, 'Patients admitted for cardiac issues may receive beta blockers only after they have been stabilized.' This underscores the need for continuous assessment to ensure that the advantages of beta blocker therapy outweigh any associated risks. The latest research reinforces the importance of personalized approaches in beta blocker therapy, particularly for older individuals, to optimize outcomes and enhance their overall well-being.
Diuretics, such as furosemide and bumetanide, play a vital role in helping individuals with cardiac issues manage fluid retention, particularly among older adults. These medications work by enhancing urine production, which can alleviate swelling and improve respiratory function. Given that older adults are more susceptible to dehydration and its related side effects, it is essential to monitor electrolyte levels and kidney function closely. Current guidelines recommend regular assessments of serum electrolytes, especially potassium and sodium, to prevent imbalances that may lead to serious complications.
Nephrologists highlight the importance of adjusting diuretic dosages based on daily weight changes, which can indicate fluid retention or loss. For example, a rapid weight gain of 2 kg over two days may signal hypervolemia, prompting immediate consultation with healthcare providers. Recent findings from 2025 underscore the effectiveness of diuretics in alleviating symptoms of fluid overload, with research showing notable decreases in weight and enhanced quality of life for older individuals with cardiac issues.
Real-world experiences illustrate the positive impact of diuretics: individuals who previously resisted conventional treatments have found significant symptom relief and weight reduction after starting customized diuretic regimens. This underscores the essential role of heart failure drugs, particularly diuretics, in the comprehensive management of cardiac conditions, ensuring that older individuals receive effective and safe treatment.
Furthermore, the recent FDA approval of Lasix ONYU, a drug-device combination for treating edema in individuals with chronic heart failure, marks an important advancement in heart failure drugs therapy. It is also crucial to consider the high prevalence of renal impairment in individuals with CHF, as this condition is associated with an increased risk of diuretic resistance when using heart failure drugs. Additionally, the potential influence of NSAIDs on diuretic effectiveness should not be overlooked, as many older individuals may be taking multiple medications. Lastly, maintaining sodium intake below 100 mmol/day is vital to prevent postdiuretic sodium retention, ensuring optimal diuretic therapy.

Sacubitril/valsartan, known as Entresto, represents a significant advancement in the treatment of cardiac dysfunction, particularly for our senior patients. This innovative therapy combines an angiotensin receptor blocker with a neprilysin inhibitor, resulting in notable improvements in heart function and a reduction in hospitalizations. Recent studies indicate that Entresto can lower the risk of initial and subsequent hospitalizations due to cardiovascular failure and related deaths by 20% to 24% compared to traditional therapies like enalapril. In real-world settings, patients treated with Entresto have demonstrated improved left ventricular ejection fraction (LVEF) and lower rates of heart failure-related events, underscoring its effectiveness in enhancing cardiovascular health among older adults.
However, it’s essential to monitor patients closely during the initial phase, as elderly individuals may experience hypotension and changes in renal function. Cardiologists stress the importance of regular renal assessments, especially since renal impairment can be more prevalent in this age group. By keeping a close eye on these factors, we can help ensure that the benefits of Entresto are maximized while minimizing potential risks, reinforcing its status as a preferred treatment option for cardiac issues in older adults.
Heart failure drugs are needed as heart failure affects nearly 6 million Americans and is the leading cause of hospitalization for those over 65, with prevalence rates reaching up to 20% among individuals over 75. Despite the benefits, only 14.3% of patients were on sacubitril/valsartan at follow-up, highlighting the need for improved adherence strategies. Additionally, patients receiving sacubitril/valsartan experienced a 33% reduction in repeat hospitalizations for cardiac problems.
Integrating Amavita's CardioElite™ SNF Program can further enhance these outcomes by offering advanced diagnostic tools and seamless care coordination. This approach not only transforms cardiac management but also significantly reduces readmissions by 93% and saves over $200K annually. If you or a loved one are navigating these challenges, know that support is available, and reaching out can make a difference in your journey to better heart health.

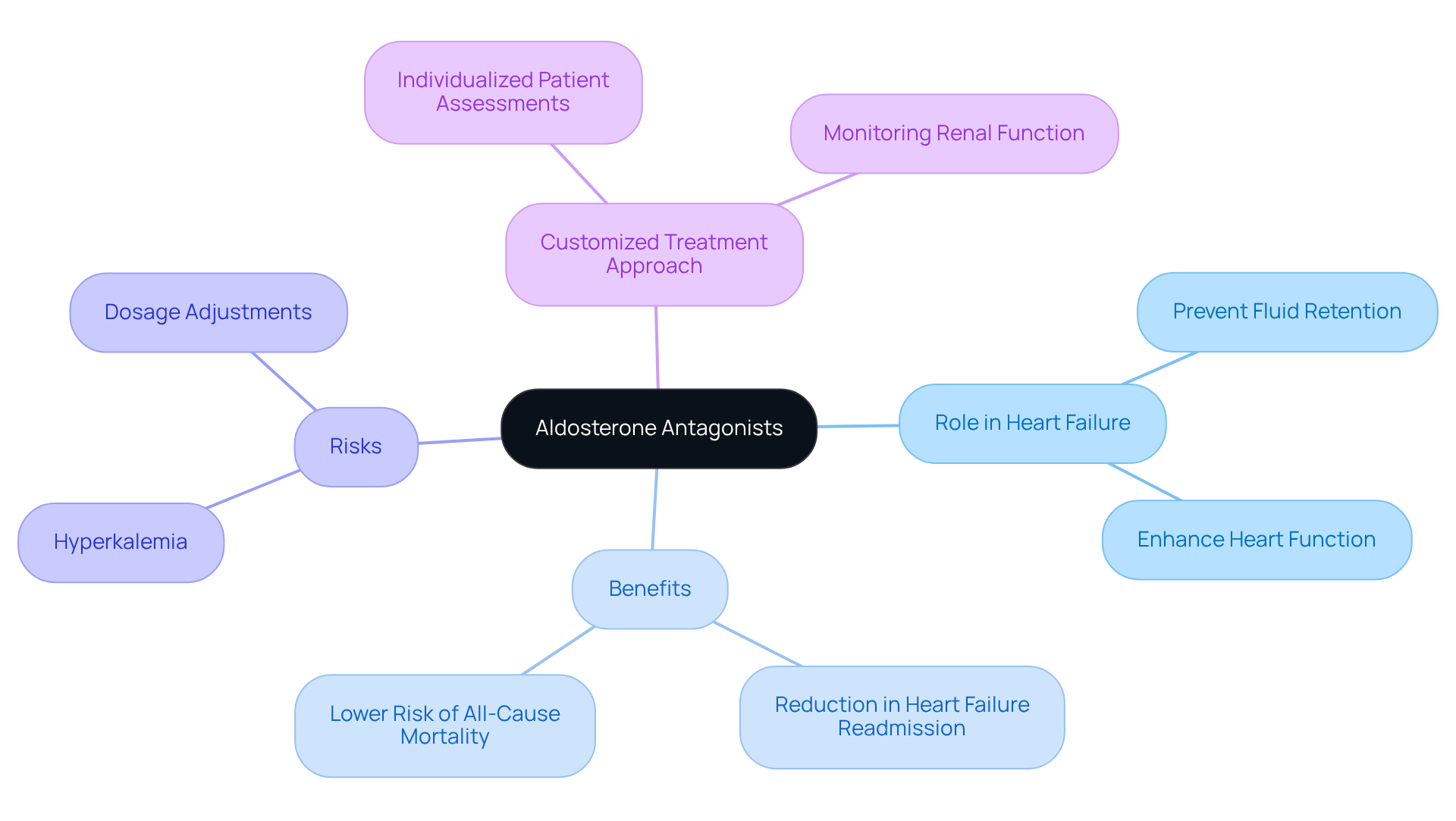
Aldosterone blockers, such as spironolactone and eplerenone, are important heart failure drugs that play a vital role in treating cardiac failure, particularly for those with reduced ejection fraction. These heart failure drugs help prevent fluid retention and enhance heart function, addressing a significant concern for many patients.
At Amavita Heart and Vascular Health, we truly understand that individuals at high risk, including the elderly, greatly benefit from thorough assessments and advanced imaging capabilities.
Monitoring potassium levels is crucial, as these medications can lead to hyperkalemia. Therefore, adjusting dosages based on renal function is essential to ensure both safety and efficacy.
Our customized approach guarantees that each individual's treatment plan is thoughtfully designed to meet their specific needs, ultimately enhancing overall cardiovascular care. We are here to support you every step of the way.
SGLT2 inhibitors, such as empagliflozin and dapagliflozin, are increasingly recognized as effective heart failure drugs for treating cardiovascular failure, especially for those at high risk, including individuals with diabetes, hypertension, or a family history of these conditions. These medications work by promoting glucose excretion and alleviating fluid overload, resulting in significant improvements in heart function. At Amavita Heart and Vascular Health, we are dedicated to providing targeted cardiovascular care, ensuring that senior individuals receive comprehensive evaluations and advanced imaging tailored to their unique treatment plans.
For elderly patients, the benefits of SGLT2 inhibitors go beyond just managing blood sugar levels; they also significantly enhance cardiovascular outcomes. Recent research has shown that dapagliflozin greatly reduces the risk of cardiovascular-related hospitalizations and mortality in older adults, demonstrating its effectiveness in real-world settings.
Studies indicate that SGLT2 inhibitors can improve diastolic function and decrease the chances of hospitalization due to cardiovascular issues, establishing them as a vital option for treating conditions with preserved ejection fraction (HFpEF). In the EMPEROR-Preserved trial, empagliflozin was associated with a notable reduction in the combined risk of cardiovascular death or hospitalization due to heart-related problems, underscoring its therapeutic potential.
Experts highlight the importance of incorporating SGLT2 inhibitors into treatment plans for older adults. Specialists note that these agents are generally well tolerated in frail older individuals, offering numerous benefits beyond glucose control. However, it is essential to monitor for potential side effects, such as urinary tract infections and dehydration, particularly in this population.
The growing body of evidence supports the use of heart failure drugs, including SGLT2 inhibitors, as a crucial component in managing cardiovascular issues for older individuals, especially those with diabetes, high blood pressure, or a family history of cardiac conditions. Their ability to improve heart function while minimizing risks makes them an essential part of modern cardiovascular care at Amavita. We are here to support you every step of the way, ensuring that you receive the best possible care tailored to your needs.

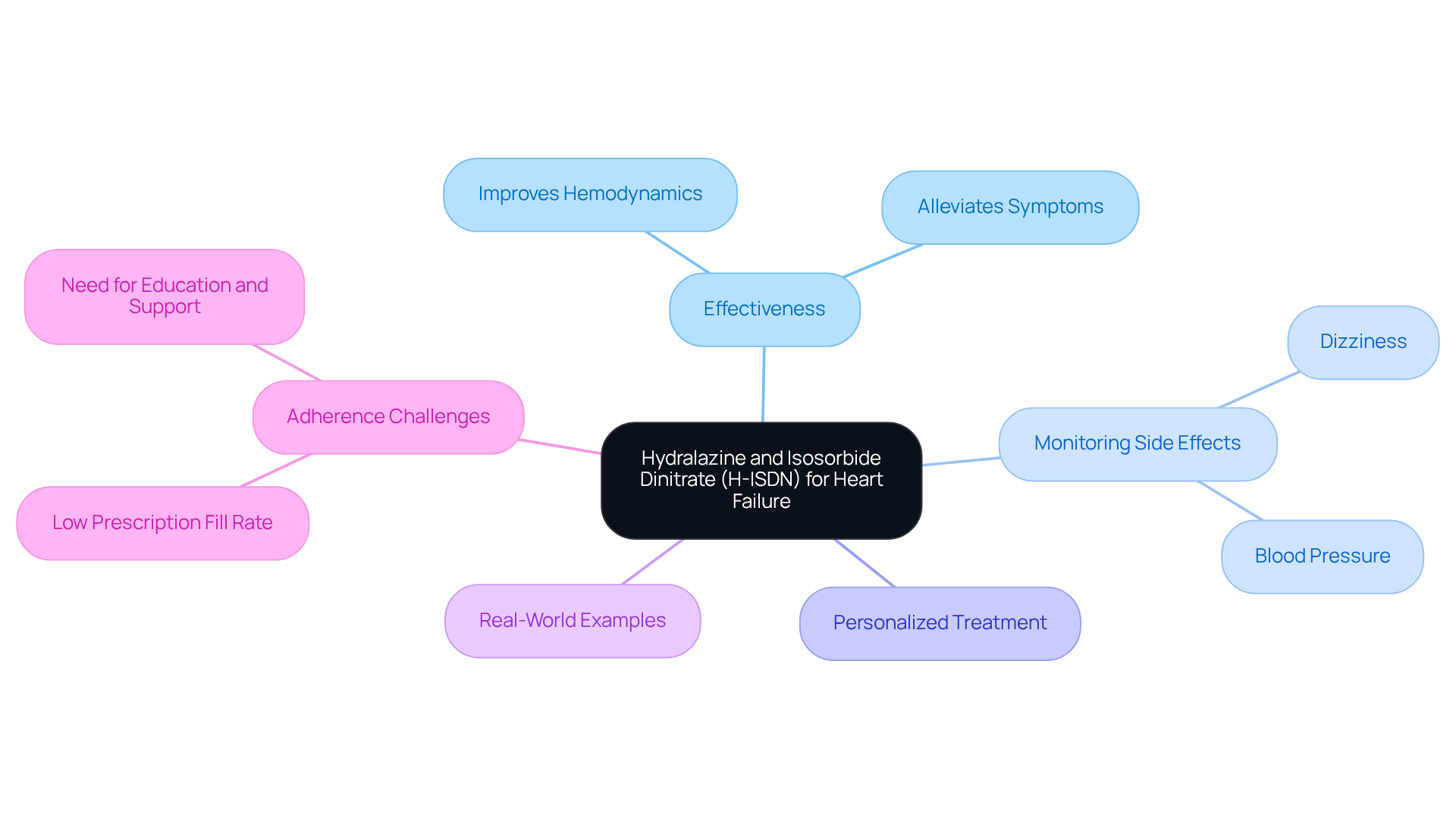
Hydralazine and isosorbide dinitrate (H-ISDN) provide important alternative options for managing cardiac dysfunction, especially for those who may struggle with ACE inhibitors or angiotensin receptor blockers (ARBs). This combination therapy has proven effective in alleviating symptoms and reducing hospitalizations for individuals taking heart failure drugs. Recent studies indicate that H-ISDN can significantly improve hemodynamics by lowering preload and afterload, which is essential for enhancing cardiac output in older adults.
For our older loved ones, it is crucial to carefully monitor blood pressure and be aware of potential side effects, such as dizziness—reported by nearly 30% of H-ISDN users. This mindfulness ensures safe and effective treatment. Cardiologists emphasize the importance of personalized treatment strategies, particularly for seniors who may have multiple health concerns. As one expert noted, "Hydralazine is an appealing choice among heart failure drugs for individuals who cannot tolerate other heart failure medications, offering a vital alternative in their management strategy."
Real-world examples highlight the successful application of H-ISDN in elderly individuals, showcasing its role in enhancing quality of life and functional capacity. However, despite its benefits, adherence to H-ISDN therapy can be challenging; studies reveal that only 3% of eligible patients fill prescriptions after discharge. This underscores the need for healthcare practitioners to focus on education and support for older adults, helping them navigate their cardiovascular challenges with confidence and care.
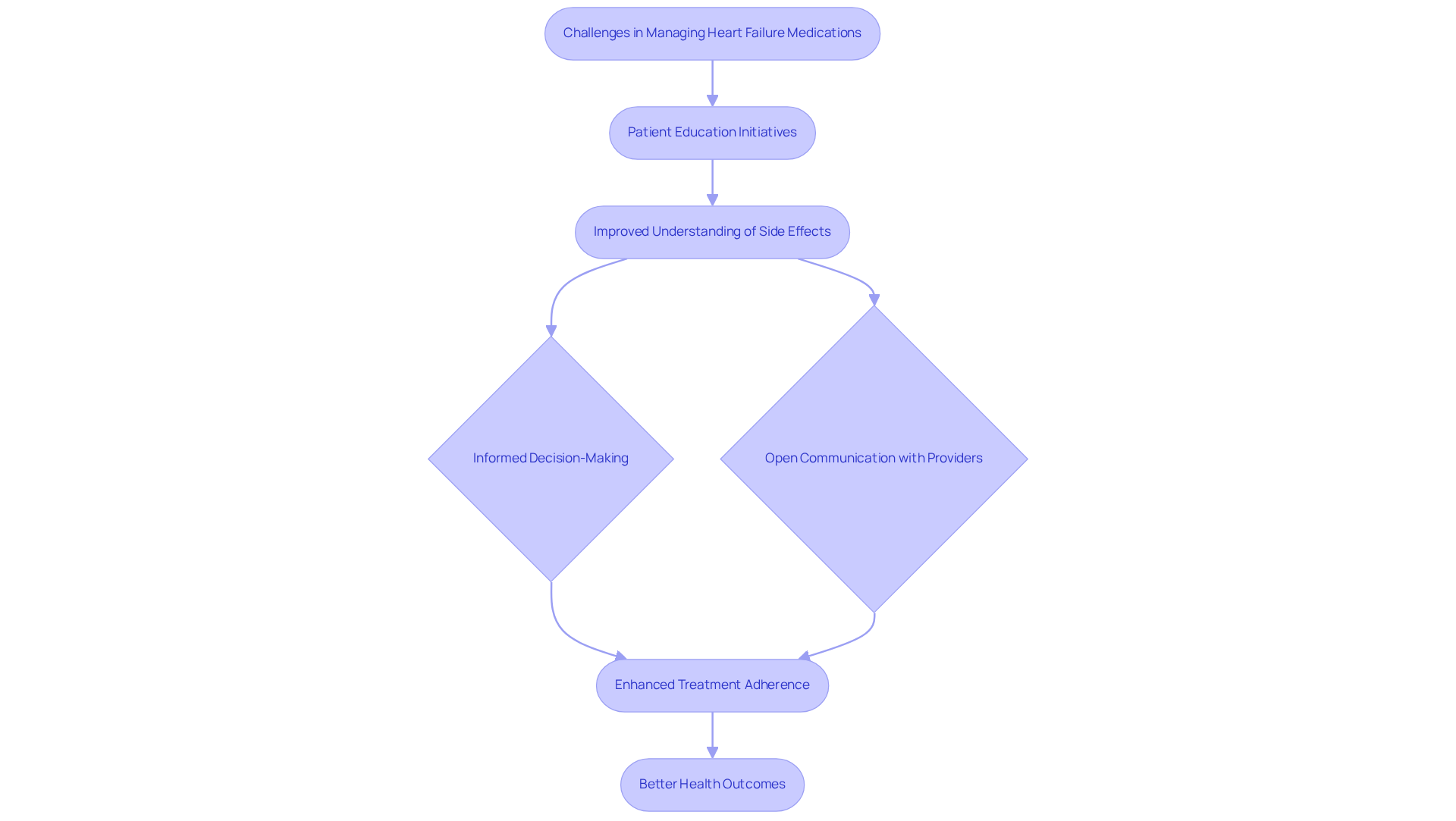
Effectively managing heart failure drugs can feel overwhelming, especially when considering their potential side effects, such as dizziness, fatigue, and gastrointestinal issues. It’s important to know that patient education is a key part of this journey. By empowering individuals and their families to recognize and report these side effects promptly, we can foster a supportive environment. For instance, when individuals are informed about the possibility of dizziness from beta-blockers, they can share their experiences with healthcare providers, leading to timely adjustments in their treatment plans.
Recent research highlights the importance of educational interventions in helping individuals understand the risks and benefits of their medications. Programs like the Strategic Memory Advanced Reasoning Training (SMART) have shown promising results. In fact, 42.5% of participants in the SMART group who initially did not meet the criteria for informed decision-making were able to do so at the 6-month follow-up. This proactive approach not only enhances communication between individuals and their providers but also contributes to better management of heart failure drugs and symptoms.
Healthcare providers stress the significance of clear communication regarding medication side effects. As Dr. Susan J. Blalock, a PhD in Pharmaceutical Outcomes and Policy, pointed out, "Informing individuals about their medications is crucial for building trust and making them feel at ease discussing any concerns." This collaborative relationship is essential for optimizing treatment outcomes and improving the overall quality of care.
Integrating healthcare education into routine care can significantly impact adherence to treatment plans. When patients understand the side effects of their heart failure drugs, they are more likely to adhere to their prescribed therapies, which helps reduce the risk of complications and hospital readmissions. Ongoing education, tailored to individual needs, is vital for navigating the complexities of cardiac management and ensuring that individuals remain engaged in their care. Regular blood tests to monitor medication effects and side effects should also be highlighted as part of this educational process. Patients are encouraged to openly discuss their experiences and any concerns with their healthcare providers to ensure the best possible management of their treatment.
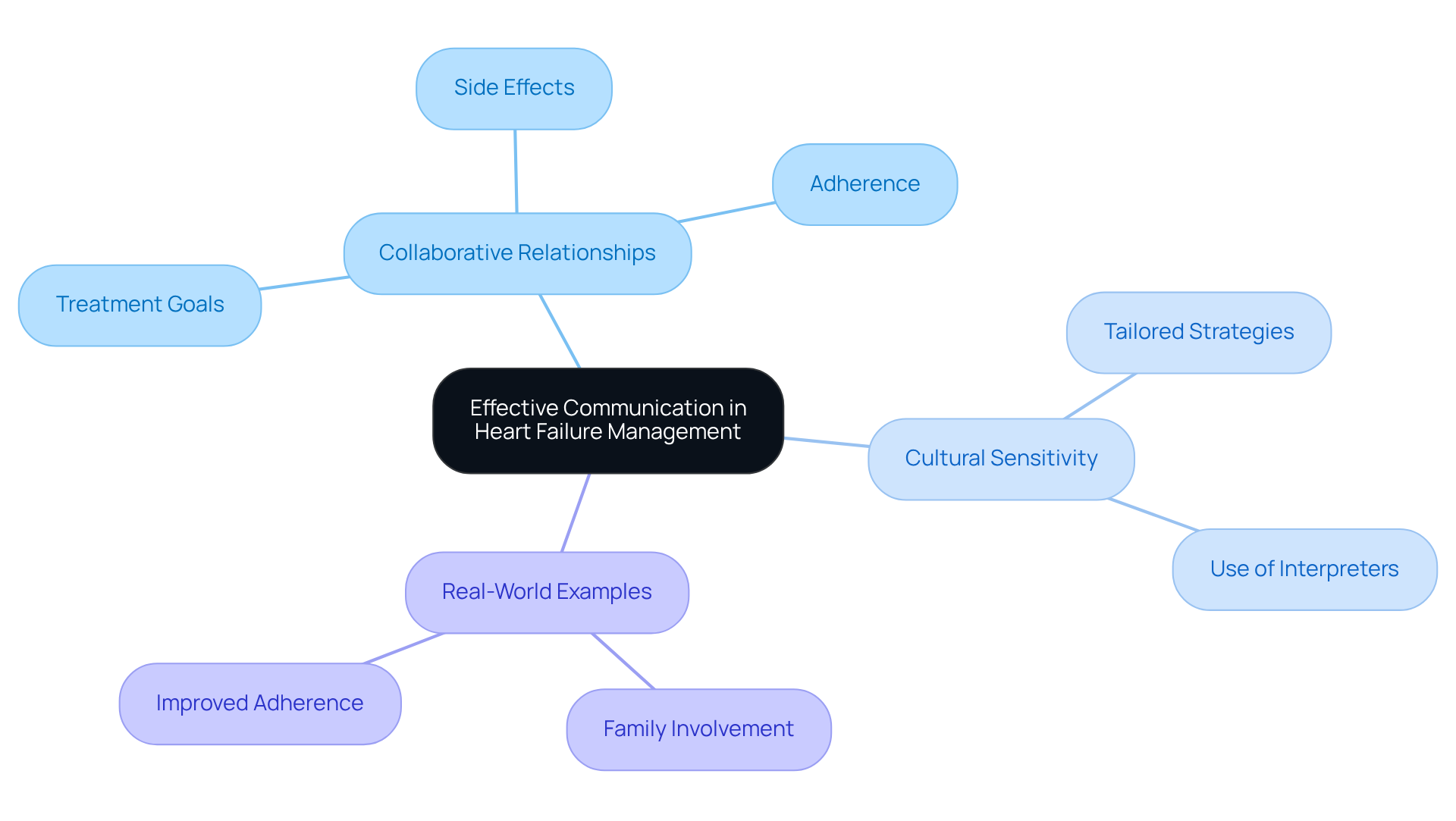
Effective communication between healthcare providers and individuals is essential for successfully managing heart failure drugs. This involves not only discussing treatment goals and potential side effects but also emphasizing the importance of adhering to prescribed regimens. In 2025, the latest strategies for enhancing provider-client communication focus on cultivating a collaborative relationship that encourages open dialogue about treatment choices and specific client requirements.
Culturally sensitive communication plays a pivotal role in enhancing understanding among diverse populations. By recognizing and valuing cultural differences, healthcare providers can tailor their communication strategies to meet the distinct needs of every individual. For instance, utilizing interpreters or culturally appropriate materials can significantly enhance understanding and engagement.
Real-world examples highlight the impact of culturally sensitive communication in the use of heart failure drugs. In one instance, a healthcare team created a program that involved family members in discussions about treatment strategies, leading to improved adherence rates among individuals from various cultural backgrounds. This approach not only empowered individuals but also fostered a supportive atmosphere conducive to better health outcomes.
Experts in healthcare communication stress the importance of these strategies. They note that effective communication can bridge gaps in understanding, ultimately leading to increased satisfaction and improved clinical outcomes. By prioritizing culturally sensitive communication, healthcare providers can ensure that all patients receive the heart failure drugs and support they need to effectively manage their condition.
At the heart of effective heart failure management lies a diverse array of medications that are essential for improving patient outcomes, especially in older adults. This article has explored ten critical heart failure drugs, highlighting their roles, benefits, and the importance of individualized treatment approaches. By understanding these medications and their impacts, patients and caregivers can better navigate the complexities of heart failure management.
Key insights discussed include:
As heart failure affects millions, it is crucial to prioritize comprehensive care strategies that not only focus on medication but also on patient education and support. By embracing a collaborative approach, individuals can take charge of their health journey, ensuring they receive the tailored care necessary for better management of their condition. Engaging with healthcare professionals, staying informed about treatment options, and actively participating in care decisions are vital steps toward enhancing quality of life for those facing heart failure challenges. Remember, you are not alone in this journey; support is always available to help you navigate your path to better health.
What is Amavita Heart and Vascular Health's approach to heart failure management?
Amavita Heart and Vascular Health employs a comprehensive approach that integrates advanced medical practices with compassionate support, creating personalized treatment strategies tailored to the specific needs of each patient, particularly elderly individuals facing multiple health challenges.
What recent advancements in heart failure treatment are mentioned in the article?
The article mentions the FDA's approval of heart failure drugs like finerenone for cardiac insufficiency with preserved ejection fraction as a significant advancement in treatment options.
How do ACE inhibitors benefit patients with heart failure?
ACE inhibitors, such as lisinopril and ramipril, help relax blood vessels, reduce the workload on the heart, and improve blood flow. They are associated with an 11% decrease in all-cause mortality and a 14% decrease in cardiovascular mortality, as well as lower hospitalization rates related to cardiac issues.
Who are the primary candidates for ACE inhibitor therapy?
Current guidelines recommend ACE inhibitors for individuals with heart failure and reduced ejection fraction, particularly those with a history of myocardial infarction, which is essential for older adults managing multiple health challenges.
What role do beta blockers play in heart failure management?
Beta blockers, such as carvedilol and metoprolol, are crucial for managing cardiac symptoms by reducing pulse rate and lowering blood pressure, leading to improved heart function and relief from symptoms like fatigue and shortness of breath.
What are the outcomes associated with the use of beta blockers in older adults?
Research shows that beta blockers can significantly enhance the quality of life and have been associated with a 25% relative decrease in all-cause mortality. A multicenter cohort study indicated a 36% reduction in mortality two years after a myocardial infarction for those treated with beta blockers.
What considerations should be taken into account when prescribing beta blockers to older patients?
Careful titration of beta blockers is essential to minimize potential side effects, and continuous assessment is necessary to ensure that the benefits of therapy outweigh any associated risks.
How does Amavita Heart and Vascular Health support patients with heart failure?
Amavita focuses on empowering patients through education and support, fostering a collaborative environment, and providing tailored cardiovascular care to enhance their overall wellness and quality of life.