


Cardioversion is an important medical procedure designed to restore a normal heart rhythm in patients experiencing arrhythmias. This procedure can significantly enhance your quality of life and reduce the risk of serious complications, such as stroke. If you or a loved one are facing concerns about heart rhythm issues, know that you are not alone. Many patients share similar worries, and it’s completely natural to feel anxious about these health matters.
The article emphasizes the value of both electrical and pharmacological methods in cardioversion. These approaches have proven effective in helping many individuals regain a sense of normalcy in their lives. However, it’s essential to understand that careful preparation and attentive post-procedure care are crucial for ensuring successful outcomes. In addition to this, having a supportive healthcare team can make a significant difference in your experience.
If you have questions or need further information, we encourage you to reach out for support. You deserve to feel informed and cared for as you navigate your health journey. Remember, taking steps towards understanding your treatment options is a positive move towards better health. We are here to help you every step of the way.
Cardioversion is a crucial procedure for managing heart rhythm disorders, especially for those facing challenges with arrhythmias like atrial fibrillation. By delivering a controlled shock to the heart, this intervention seeks not only to restore a normal rhythm but also to ease the distressing symptoms that can affect daily life.
However, as the complexities of heart health unfold, you may wonder: how can patients navigate the intricacies of preparation, procedure, and recovery to achieve the best possible outcomes?
This article explores the essential steps and considerations of cardioversion, guiding you on the path to reclaiming heart health and enhancing your quality of life.
Cardioversion is a vital medical intervention focused on shocking the heart back into rhythm for individuals experiencing arrhythmias, such as atrial fibrillation or atrial flutter. The primary goal is shocking the heart back into rhythm to restore an irregular heart pattern to a normal sinus rhythm, alleviating distressing symptoms like palpitations, shortness of breath, and fatigue. This procedure is especially important for older adults, who may be at greater risk for complications such as stroke and heart failure, particularly if they have underlying conditions like diabetes or hypertension.
Did you know that atrial fibrillation accounts for one in seven strokes in the United States? This statistic underscores the critical need for timely intervention. Cardioversion enhances immediate health outcomes and significantly improves overall quality of life by shocking the heart back into rhythm. Research indicates that shocking the heart back into rhythm can lead to a notable reduction in symptoms and a greater sense of well-being among patients.
Cardiologists emphasize that for older adults with arrhythmias, this procedure is more than just a treatment; it represents a pathway to reclaiming vitality and independence. It allows individuals to engage more fully in daily activities and enjoy an enriched quality of life. At Amavita Heart and Vascular Health, we are dedicated to comprehensive arrhythmia management. Our approach incorporates advanced imaging and minimally invasive techniques to ensure the best possible outcomes.
Furthermore, we utilize continuous monitoring technology to identify specific types of arrhythmias and provide advanced treatments that restore the heart's natural rhythm. With atrial fibrillation affecting approximately 2 million Americans, the significance of shocking the heart back into rhythm to prevent serious complications cannot be overstated. Our CardioElite™ program enhances cardiac care by providing real-time diagnostic information and expert consultation, ensuring that high-risk individuals receive the targeted care they need. We are here to support you on this journey towards better heart health.

Cardioversion is an important procedure that can be categorized into two main types: electrical and pharmacological.
Electrical conversion involves delivering a controlled electric shock to the heart, shocking the heart back into rhythm through paddles or electrodes placed on the chest. This method is often preferred in emergency situations or when it’s crucial for shocking the heart back into rhythm quickly. It has a remarkable success rate of over 90%, especially for those who are hemodynamically compromised due to new-onset atrial fibrillation (AF) or atrial flutter (AFL). As cardiologist Axel Brandes points out, "Electrical conversion of heart rhythm terminates AF in over 90% of cases and is the preferred treatment for severely compromised patients with new-onset AF or AFL."
On the other hand, pharmacological intervention involves using medications to restore normal heart function. This approach typically requires more time to achieve results. Common antiarrhythmics, such as amiodarone and flecainide, can convert recent-onset or paroxysmal AF to sinus rhythm in 50-70% of cases. However, the effectiveness of these medications can vary based on factors like the duration of AF and the specific drug used.
Both methods have their own advantages and considerations.
Interestingly, statistics suggest that a wait-and-see approach, which involves rate-control medications followed by a possible later shocking the heart back into rhythm, has shown non-inferiority to immediate restoration in achieving sinus regularity after four weeks. In a recent trial, 91% of individuals in the delayed group achieved sinus regularity, compared to 94% in the early group, underscoring the effectiveness of both methods.
Real-life experiences further illustrate the success of shocking the heart back into rhythm. For instance, one individual with persistent AF underwent this intervention and successfully restored normal rhythm, significantly improving their quality of life.
Cardiologists emphasize that choosing between electrical and pharmacological methods should be tailored to the individual’s unique condition, urgency of treatment, and overall health status, ensuring the best possible outcomes. Remember, you are not alone in this journey; support is available to help you navigate your heart health.

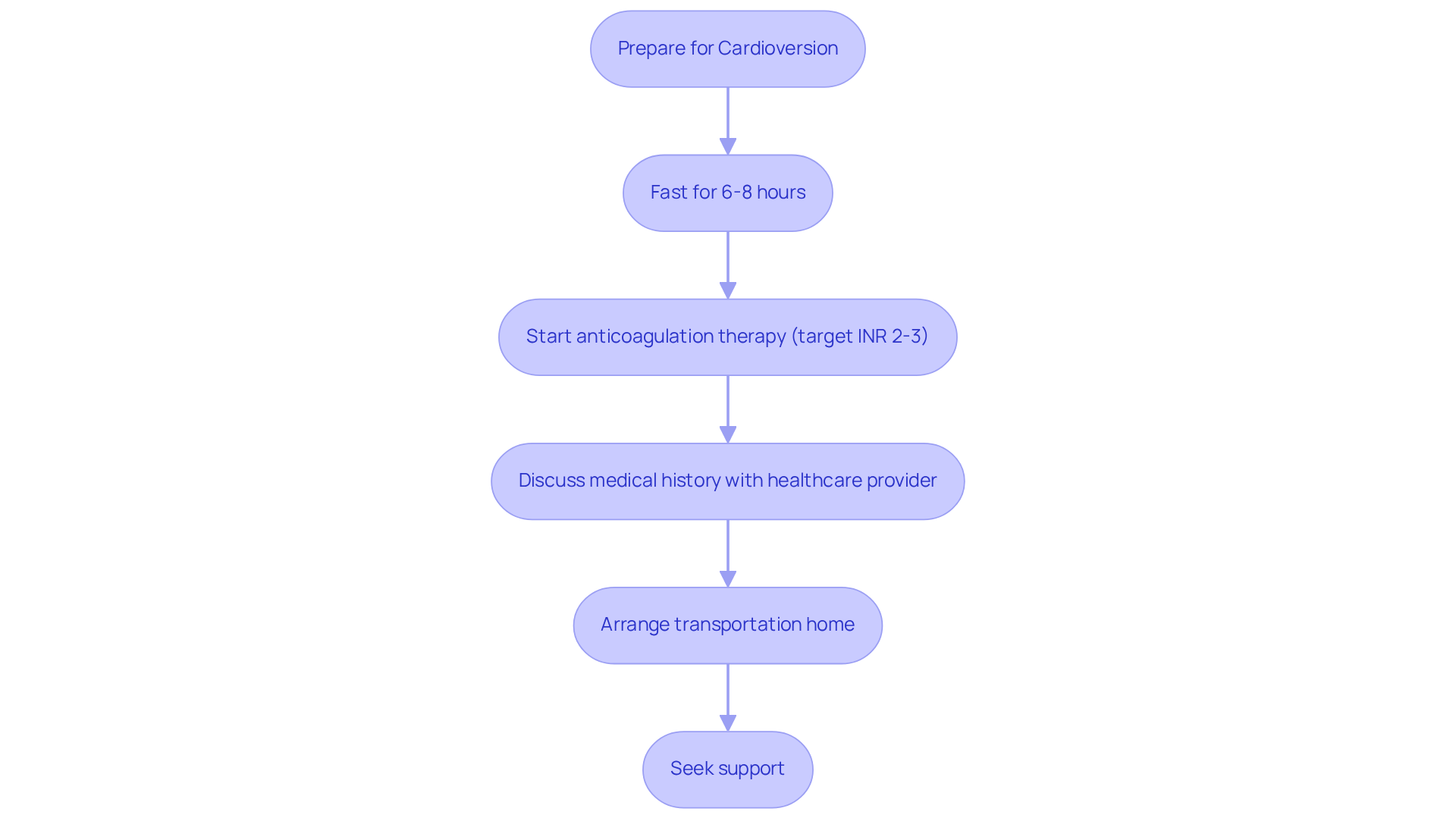
Preparing for an electrical conversion involves several crucial steps that prioritize your safety and well-being. It’s common for patients to be advised to fast for at least 6-8 hours before the procedure. This is to help minimize any risks associated with sedation. Additionally, anticoagulant medications are essential in preventing blood clots, especially for those who have experienced atrial fibrillation over time. Current guidelines suggest starting anticoagulation therapy with a target INR of 2-3 for a minimum of three weeks before and four weeks after cardioversion. This approach significantly lowers the risk of stroke, providing peace of mind.
Engaging in open conversations with your healthcare provider about your medical history, current medications, and any allergies is equally important. Such discussions ensure that all potential risks are addressed and that your treatment plan is tailored to your unique needs. It’s also wise to arrange for someone to drive you home after the procedure, as you will be under sedation and unable to drive safely.
Real-life experiences underscore the importance of these preparations. For instance, an individual who underwent heart rhythm restoration while on blood thinners shared a smooth recovery, highlighting the reassurance that comes from adhering to pre-procedure guidelines. Healthcare professionals consistently stress that effective anticoagulation and clear communication are vital for achieving successful outcomes in shocking the heart back into rhythm. Remember, you are not alone in this journey; support is always available to help you through.
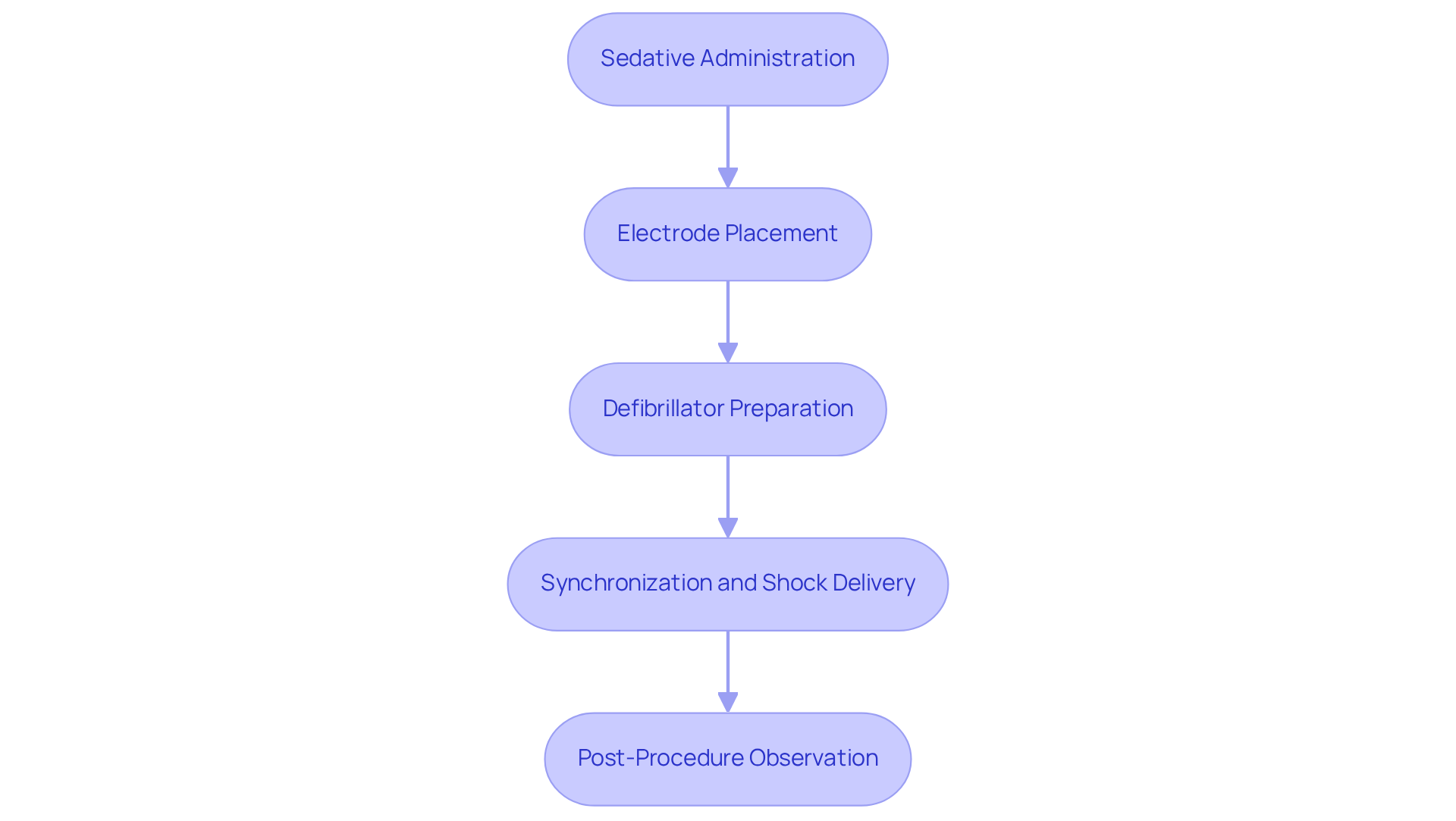
During the electrical cardioversion procedure, it’s natural to have concerns about safety and comfort. That’s why individuals are closely monitored in either a hospital or outpatient setting. Initially, a sedative is given to help everyone relax, creating a more comfortable environment. Once sedated, electrodes are gently placed on the chest, and the defibrillator is prepared to deliver a low-energy shock to the heart. This shock is synchronized with the heart's rhythm, optimizing its effectiveness and typically lasting only a few minutes.
After these steps are carried out, individuals are observed for at least an hour. This observation period is crucial for assessing the effectiveness of the cardioversion and for managing any possible side effects, such as skin irritation from the electrodes. For older individuals, special attention is given to their unique health considerations. They may face a procedural mortality rate of approximately 0.2%, which underscores the importance of a multidisciplinary approach in managing their care. By addressing any underlying conditions, we aim to minimize risks and enhance overall safety.
In general, this method is designed for shocking the heart back into rhythm efficiently while prioritizing the safety and comfort of each individual. Remember, you are not alone in this process; we are here to support you every step of the way. If you have any questions or concerns, please don’t hesitate to reach out for help.
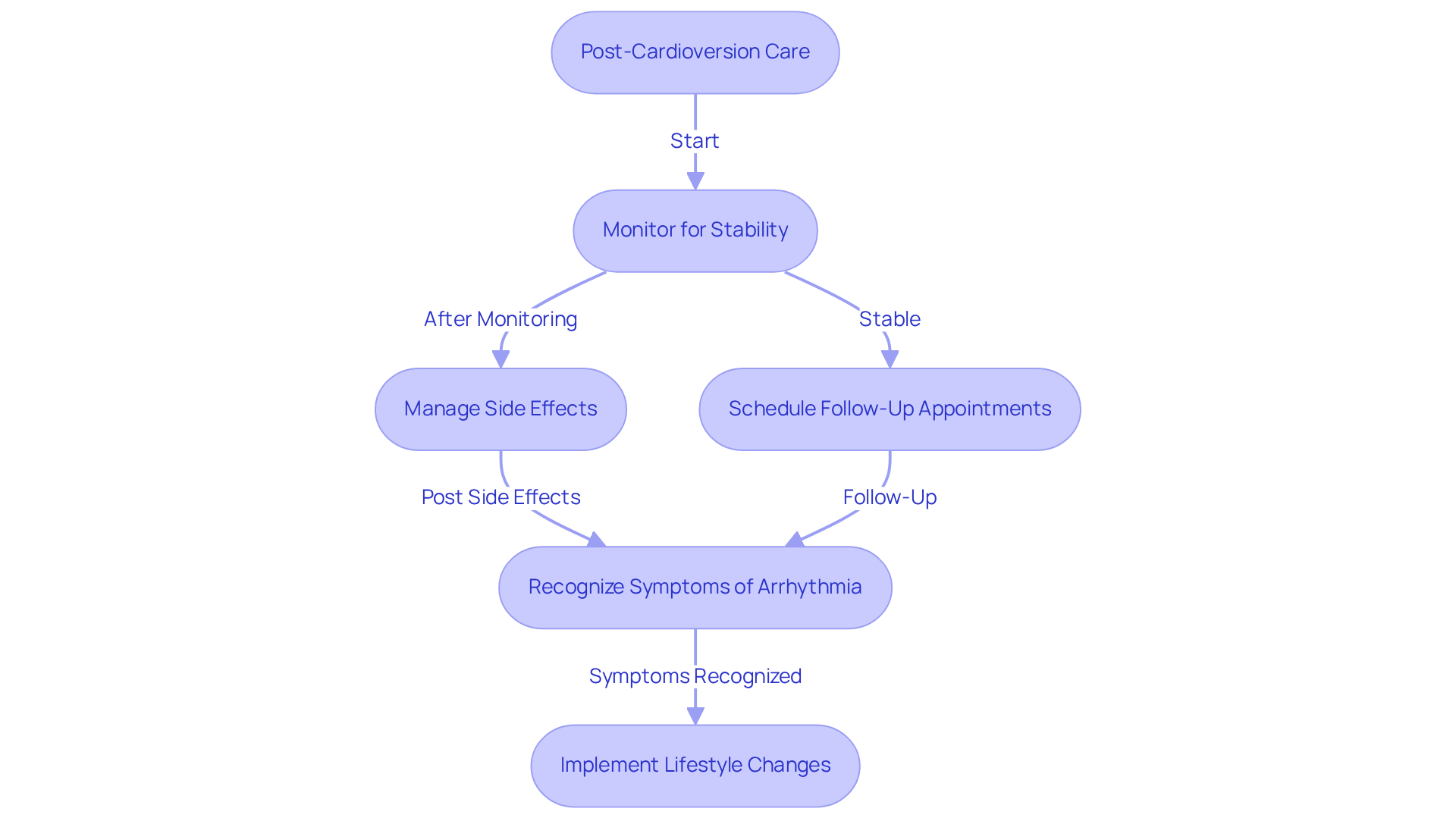
After cardioversion, it's important for individuals to be closely monitored for several hours to ensure they feel stable. You might experience some mild side effects, such as fatigue or slight discomfort at the electrode sites, which can feel similar to sunburn. To support your recovery, please remember to avoid strenuous activities for at least 24 hours following the procedure.
Follow-up appointments are essential in assessing your heart's rhythm and determining whether further treatments or medications might be necessary. It’s also vital to be aware of any symptoms that could indicate arrhythmia recurrence, like dizziness or an irregular heartbeat, and to know when to seek medical help.
By sticking to your prescribed medications and making lifestyle changes—such as adopting a heart-healthy diet and engaging in regular exercise—you can significantly enhance the long-term success of your cardioversion. This not only promotes your health but also contributes to a better quality of life. Remember, you are not alone in this journey; support is always available to help you through.
Cardioversion is essential in managing heart rhythm disorders, particularly arrhythmias like atrial fibrillation and atrial flutter. This procedure, whether electrical or pharmacological, aims to restore the heart's normal rhythm, alleviating distressing symptoms and significantly enhancing the quality of life for those affected. Understanding the significance of cardioversion is crucial for individuals, especially older adults, who may face heightened risks of complications from irregular heart rhythms.
In this article, we have explored key insights into the types of cardioversion, preparation steps, procedural details, and post-care guidelines. The distinction between electrical and pharmacological methods emphasizes the tailored approach necessary for effective treatment, ensuring that individuals receive the most appropriate care based on their unique health needs. The focus on preparation and follow-up care highlights the importance of a comprehensive strategy in achieving successful outcomes and maintaining heart health.
Ultimately, the journey toward better heart health begins with awareness and proactive management of arrhythmias. Are you ready to engage in open dialogues with your healthcare provider? By adhering to treatment plans and making lifestyle adjustments that support heart health, you can significantly reduce the risks associated with arrhythmias and reclaim a vibrant, active life. Remember, you are not alone on this journey; support is available, and taking these steps can lead to a brighter, healthier future.
What is cardioversion and why is it important?
Cardioversion is a medical intervention that aims to restore an irregular heart rhythm to a normal sinus rhythm, particularly for individuals experiencing arrhythmias like atrial fibrillation or atrial flutter. It is crucial for alleviating distressing symptoms such as palpitations, shortness of breath, and fatigue, especially in older adults who are at higher risk for complications like stroke and heart failure.
What are the two main types of cardioversion?
The two main types of cardioversion are electrical and pharmacological. Electrical conversion involves delivering a controlled electric shock to the heart, while pharmacological conversion uses medications to restore normal heart function.
How does electrical cardioversion work?
Electrical cardioversion delivers a controlled electric shock to the heart through paddles or electrodes placed on the chest. It is often used in emergency situations and has a success rate of over 90%, particularly for patients who are hemodynamically compromised due to new-onset atrial fibrillation or atrial flutter.
What is pharmacological cardioversion?
Pharmacological cardioversion involves using medications, such as antiarrhythmics, to restore normal heart rhythm. This method typically takes longer to achieve results and can convert recent-onset or paroxysmal atrial fibrillation to sinus rhythm in 50-70% of cases.
What are the advantages and considerations of each cardioversion method?
Electrical conversion is generally safe but may have complications related to sedation and, in rare cases, ventricular fibrillation. Pharmacological conversion is less invasive but can lead to medication side effects and requires careful monitoring for thromboembolic events.
How effective is a wait-and-see approach compared to immediate cardioversion?
A wait-and-see approach, which involves using rate-control medications followed by possible later cardioversion, has shown similar effectiveness to immediate cardioversion. In a recent trial, 91% of individuals in the delayed group achieved sinus regularity after four weeks, compared to 94% in the early group.
How can individuals choose between electrical and pharmacological cardioversion?
The choice between electrical and pharmacological cardioversion should be tailored to the individual's unique condition, urgency of treatment, and overall health status, ensuring the best possible outcomes.